Medication Misunderstandings
It’s a vexing and recurrent problem.
You attend a doctor’s appointment.
You have a diagnosis or complaint we’ll refer to as the “plague.”
You may or may not already have other medical conditions.
You may or may not be on other medications.
The doctor says, “You’ve got the “plague.” We’ll try some “potion” [a.k.a., a new medication] and see what that does.” He or she quickly enters the prescription into the electronic medical record, sends the prescription to the pharmacy, says, “I’ll see you in 3 months,” and exits.
Okay.
You proceed to the pharmacy, purchase the new “potion,” and after opening the package, you pour over the 12-page insert that discusses the reasons for taking this medication along with a wide array of possible risks and side effects. (Seems harmless, right?)
It is at this point that you realize you’re already on a medication for the “plague.” Do you stop that medication before you take the new “potion”? Do you take the new “potion” in addition to the medication you’re already taking? How will you know if the new “potion” is working?
You are officially unsure about taking the “potion” because you have legitimate questions about its use, safety, benefits, and effectiveness. You wish you had asked these questions before you left the doctor’s office. Now you must now try to contact your doctor either by phone or by using the electronic medical record, neither of which are particularly attractive or constructive options.
This very situation plays out every single day for thousands of patients who receive new medication prescriptions or changes to their medication regimens.
In an article published some time ago (2012) in the Journal of General Internal Medicine [Medication Reconciliation Accuracy and Patient Understanding of Intended Medication Changes on Hospital Discharge], Horwitz, et al, studied a population of patients discharged from the hospital with medication changes. (Medical reconciliation is defined by JCAHO as “the process of comparing a patient's medication orders to all of the medications that the patient has been taking. This reconciliation is done to avoid medication errors such as omissions, duplications, dosing errors, or drug interactions.”)
Horwitz, et al, discovered medical reconciliation discharge errors occurred for several reasons:
(1) patients had no understanding of (69.3 %) of re-dosed medications,
(2) patients had no understanding of (81.6 %) stopped medications,
(3) patients had no understanding of (62.0 %) new medications, and
(4) patients experienced (24.2%) suspected provider errors.
Altogether, 81.4 % of the patients studied either experienced a provider error or had no understanding of at least one intended medication change.
Mic drop.
81.4% is a lot of patients.
“…81.4 % of the patients studied either experienced a provider error or had no understanding of at least one intended medication change.”
I would be remiss, however, if I didn’t point out that the provision of care (whether it be advances in the electronic medical record system or changes in the discharge process) has changed a lot since 2012. So, these numbers may not reflect what is actually happening in 2024. Having said that, I frequently (anecdotally) encounter medication confusion during consults with clients at Sideline MD.
The question at hand is this: how can I (as a patient) be sure that I walk away from my interaction (hospital stay, doctor’s appointment, video visit, etc.) assured that I understand my medications whether they are existing, new or even different?
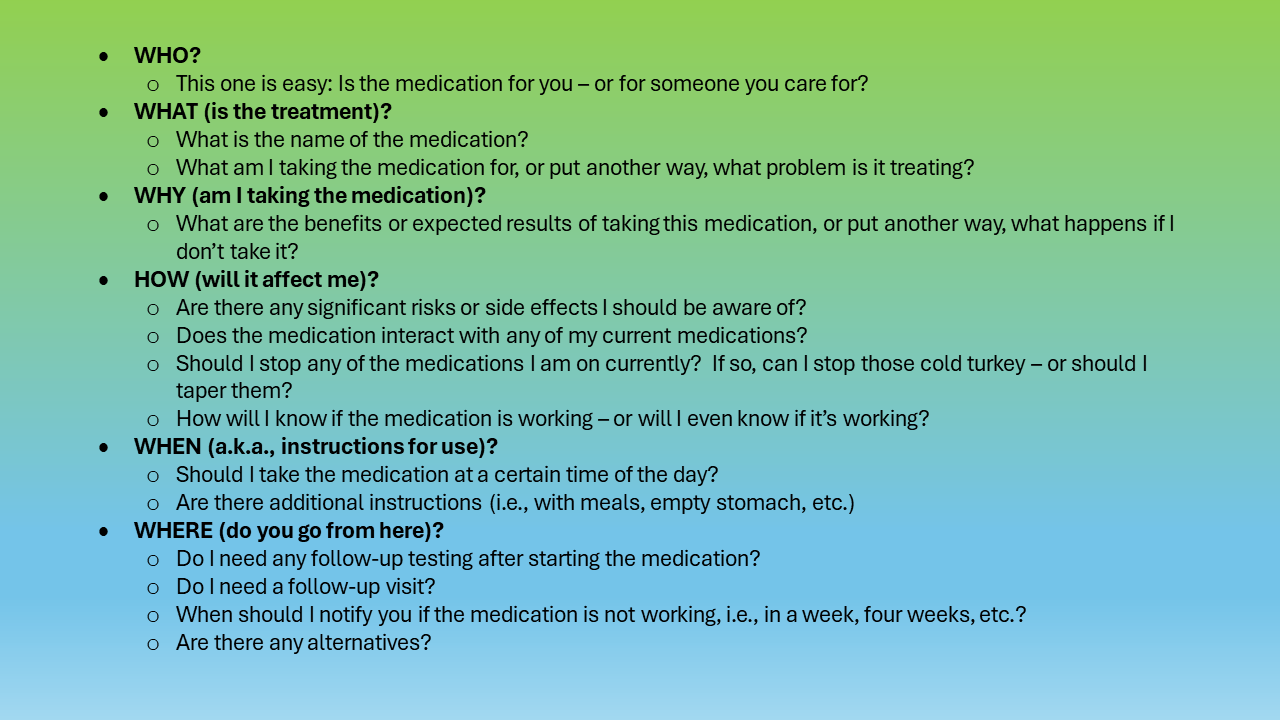
So, here is a list of questions or bullet points that I have compiled (using the 5 W’s) after having interacted with lots of clients and patients who’ve had these types of experiences and wished they would have asked more questions (NOTE: I threw the H for HOW into the mix, too.):
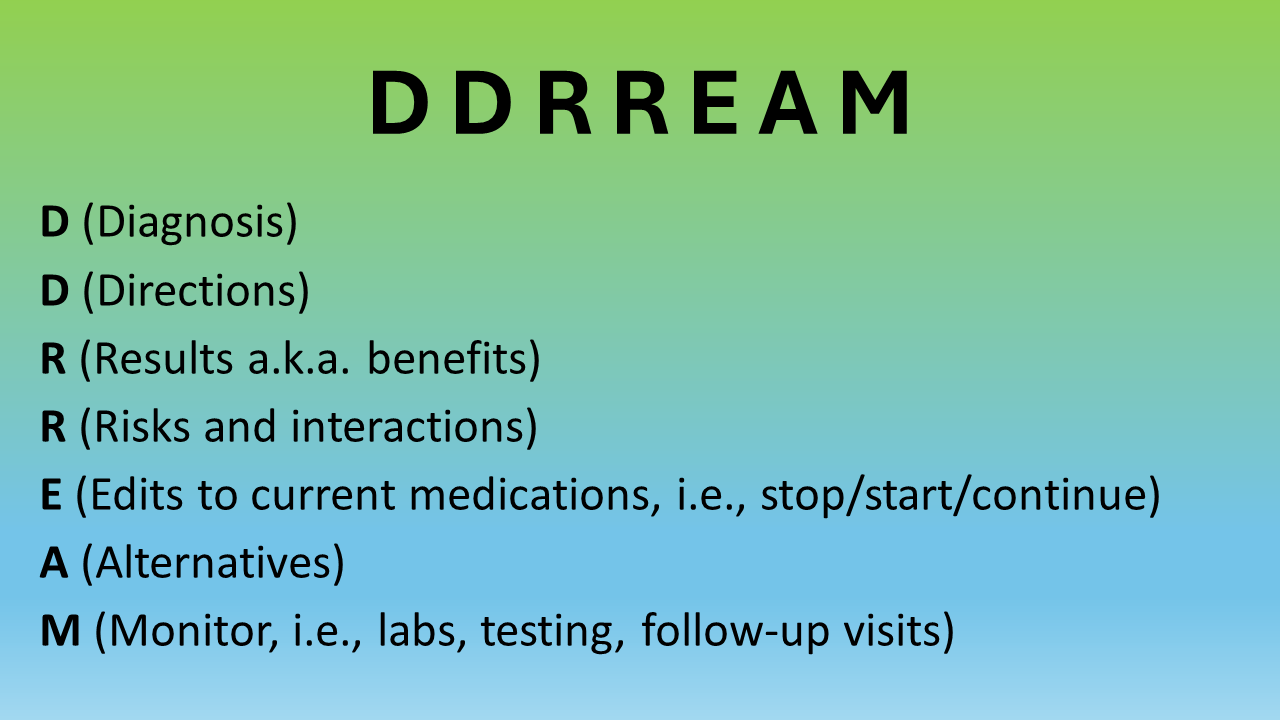
This is a lot to remember, so I will try to break it down in a different way using an acronym:
Utilizing this acronym during visits when medications are added can be very helpful in understanding your treatment plan. This acronym can be used just as easily to address situations where medications are adjusted or even discontinued – just adjust the verbiage a bit.
Lastly, I would suggest bringing a notebook with you when attending your medical visits. Keep this acronym, along with other scripting suggestions from Sideline MD, written in the notebook so that you’re ready to have a productive interaction with your physician or provider.
In my opinion, your healthcare experience is now contingent on your ability to function as a prepared and informed health citizen. In 2024, healthcare in the United States of America functions as a complicated business (sad, but true). This statement is well-researched and deserves its own series of explanations and discussions. In her book, An American Sickness, Rosenthal states, “The American health care system thrives on complexity, making it nearly impossible for patients to navigate on their own.”
Knowing this, it is our job as healthcare consumers (and health citizens) to take charge of our experiences in order to pursue improved outcomes and high-quality care. Stay tuned for more posts on how to become an informed and effective health citizen.
Thanks for reading…